Menstrual Irregularities & AUB
Medical Laboratory And Specialists Services
Menstrual irregularities refer to deviations from the normal menstrual cycle, which can manifest as variations in cycle length, flow, or symptoms. These irregularities can be a normal part of life for many, especially during adolescence, perimenopause, or due to temporary changes in health or lifestyle. However, persistent irregularities might signal underlying health issues. Here’s a note on some common types of menstrual irregularities and their possible causes:
1. Amenorrhea: Absence of menstruation.
Types: Primary Amenorrhea: Absence of menstruation by age 15 in someone who has otherwise
developed normally.
Secondary Amenorrhea: Cessation of menstruation for three or more months in someone with
previously regular cycles.
Causes: Pregnancy, hormonal imbalances, extreme weight loss, excessive exercise, stress, thyroid disorders, and certain medications or health conditions.
2. Menorrhagia: Excessively heavy or prolonged menstrual bleeding.
Causes: Uterine fibroids, polyps, hormonal imbalances (such as thyroid disorders), endometriosis, and blood clotting disorders.
3. Oligomenorrhea: Infrequent menstrual periods, typically occurring more than 35 days apart.
Causes: Polycystic ovary syndrome (PCOS), thyroid disorders, excessive stress, significant weight changes, and certain medications
4. Polymenorrhea: Frequent menstrual periods, occurring less than 21 days apart.
Causes: Hormonal imbalances, uterine abnormalities, and infections.
5. Dysmenorrhea: Painful menstruation, which can be primary (not related to pelvic pathology) or secondary (associated with conditions like endometriosis or fibroids).
Causes: Hormonal changes, pelvic inflammatory disease (PID), endometriosis, fibroids, and other pelvic conditions.
6. Spotting Between Periods: Light bleeding or spotting that occurs between menstrual periods.
Causes: Hormonal fluctuations, implantation bleeding (in early pregnancy), uterine fibroids or polyps, infections, and use of contraceptives like birth control pills or intrauterine devices (IUDs).
7. Irregular Cycles: Variability in the length of the menstrual cycle.
Causes: Stress, weight fluctuations, thyroid disorders, PCOS, and other hormonal imbalances.
Management and Treatment: Addressing menstrual irregularities often involves identifying and treating the underlying cause. Common approaches include:
Lifestyle Changes, Medication: Hormonal treatments, such as birth control pills or hormonal IUDs, can help regulate cycles, Treatment for conditions like fibroids, endometriosis, or thyroid disorders, which might require surgical or specialized medical care.
If menstrual irregularities are persistent, severe, or accompanied by other symptoms, it’s important to consult a healthcare provider for proper diagnosis and treatment. They can offer guidance based on individual health needs and conditions.
Abnormal uterine bleeding (AUB) refers to any bleeding from the uterus that deviates from normal menstrual patterns.
PALM-COEIN Classification
This system categorizes the causes of AUB into structural and non-structural categories:
PALM (Structural Causes)
1. P – Polyps: Benign growths of the endometrial lining that can cause irregular or heavy bleeding.
2. A – Adenomyosis: Condition where endometrial tissue grows into the muscular wall of the uterus, causing heavy and painful periods.
3. L – Leiomyomas (Fibroids): Benign tumors of the uterine muscle that can cause heavy bleeding, pelvic pain, or pressure symptoms.
4. M – Malignancy and Hyperplasia: Endometrial hyperplasia (thickening of the uterine lining) and cancers (endometrial or cervical).
COEIN (Non-Structural Causes)
1. C – Coagulation Disorders: Conditions that affect blood clotting, leading to heavy or irregular bleeding.
2. O – Ovulatory Dysfunction: Irregular or absent ovulation can lead to irregular bleeding or amenorrhea.
3. E – Endometrial Disorder: Disorders affecting the endometrium, such as endometrial hyperplasia without malignancy.
4. I – Iatrogenic: Bleeding caused by medical interventions or medications, such as hormonal contraceptives or anticoagulants.
5. N – Not Otherwise Classified: Any other causes of AUB that do not fit into the above categories, including certain systemic or lifestyle factors.
The management Strategies include:
1. Diagnosis: Medical History and Physical Exam: Detailed history and examination to understand
bleeding patterns and associated symptoms.
Laboratory Tests: Blood tests to assess anemia, thyroid function, and coagulation status.
Imaging: Ultrasound, hysteroscopy, or sonohysterography to evaluate uterine structure.
Biopsy: Endometrial biopsy if there is suspicion of hyperplasia or malignancy.
2. Medical Management: Hormonal Treatments: Birth control pills, hormone-releasing intrauterine devices (IUDs) to regulate or reduce bleeding.
Non-Hormonal Medications: NSAIDs for pain and to reduce bleeding, and tranexamic acid to decrease heavy bleeding.
Management of Coagulation Disorders: Specific treatment for bleeding disorders.
3. Surgical Management: Dilation and Curettage (D&C): Removal of the uterine lining for diagnostic and therapeutic purposes.
Endometrial Ablation: Procedure to destroy the uterine lining to reduce or stop bleeding.
Myomectomy or Hysterectomy: Surgical removal of fibroids or the uterus, respectively, depending on the severity and other factors.
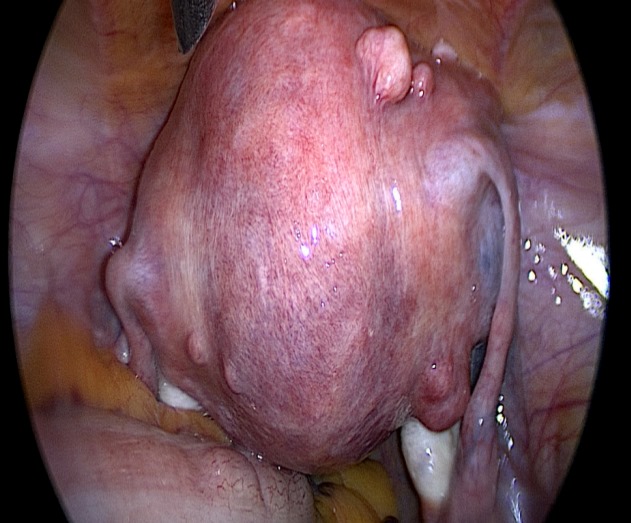
Uterus with multiple fibroid
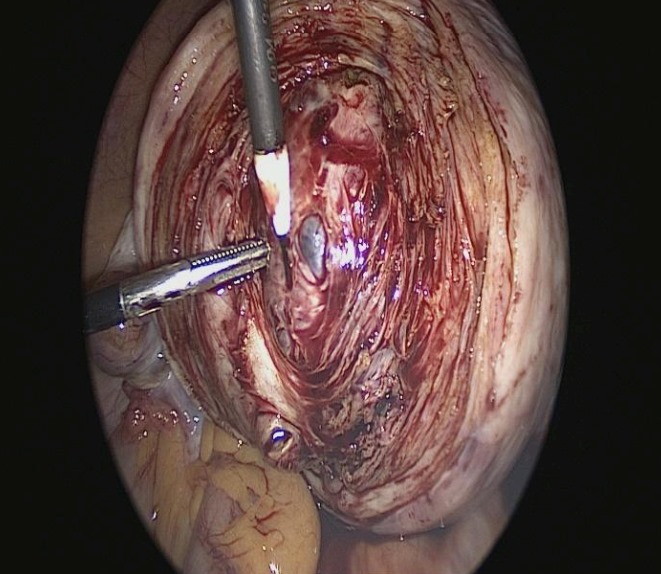
Laparoscopic Myomectomy
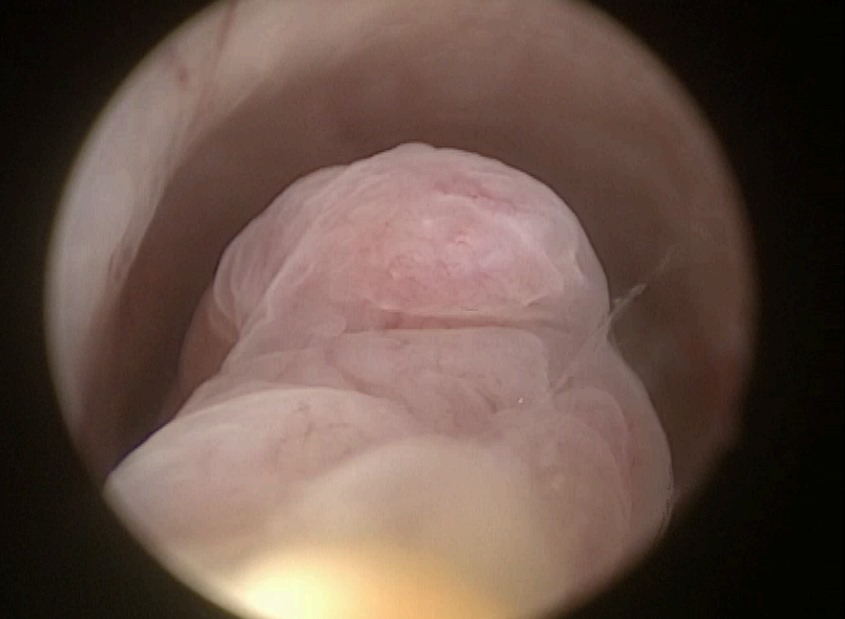
Hysteroscopy Polypectomy
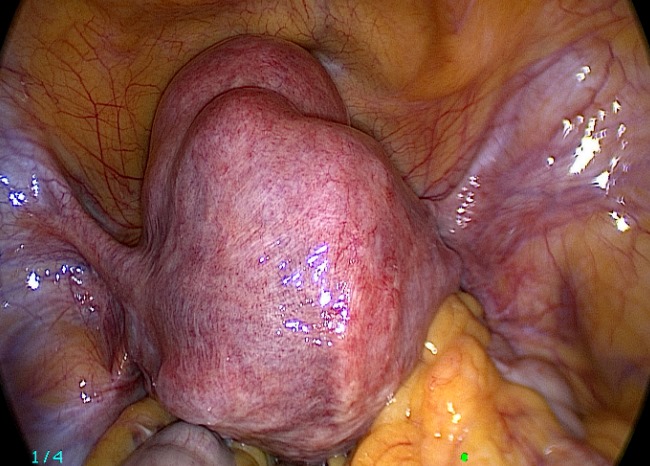
Uterus with multiple fibroid
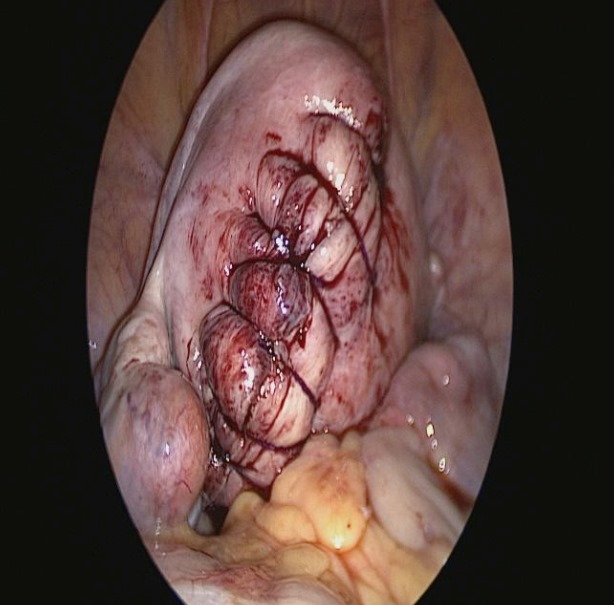
Post Myomectomy Uterine repair
