Paediatric Lower Limb Conditions
Medical Laboratory And Specialists Services
Paediatric Lower Limb Conditions
Lower limb conditions can present in various ways from pain, limp, or alignment issues to visible deformity in the child. They can either be physiological (within normal range) that do not require treatment or pathological that require treatment.
1. Alignment issues
- a. Bow legs (Genu varum)
- b. Knock knees (Genu Valgum)
- c. Intoeing
2. Limb length discrepancy (LLD)
- a. Developmental dysplasia of the hip (DDH)
- b. Slipped Capital Femoral Epiphysis (SCFE)
- c. Perthes disease of the Hip (LCPD)
4. Tibial bowing
5. Foot and ankle
- a. Clubfoot
- b. Congential Vertical talus
- c. Flatfeet
- d. Toe walking
- e. Metatarsus adductus
- f. Congenital toe deformities
1. Bow Legs (Genu Varum)
Bow legs are an outward curvature of the legs, leading to an unstable gait and uneven weight distribution. Bow legs can either be physiological (normal) or pathological. Physiological bow legs do not require treatment.

2. Knock Knees (Genu Valgum):
Knock knees involve an inward curvature of the legs, causing the knees to touch while the ankles remain apart. This condition can lead to knee pain, instability, and difficulties with walking.

Treatment of Knock Knees, Bow legs
All deformities can result from conditions such as metabolic disorders, congenital anomalies, developmental disorders, growth disturbances, trauma, or acquired deformities. Lower limb deformity correction surgery is a specialized procedure aimed at addressing structural abnormalities in the bones and joints of the leg and foot. Surgical treatment depends upon the severity of the condition, age of patient, and underlying disease process. The aim of all surgical treatment is to restore optimum function and normal anatomy.The surgical intervention can be done with guided growth / growth modulation, or corrective osteotomies and fixation with internal or external fixator.

3. Intoeing:
Often parents notice that as children begin to walk, they walk with feet turned inwards and the toes pointing towards each other. This is called intoeing or pigeon-toed. The cause can be from hips, legs, or feet. Assessment is done clinically, with the help of xrays, and CT scanogram of the lower limbs. Surgery may be required for children who have difficulty walking and performing activities of daily living.
4. Limb Length Discrepancy:
Limb length discrepancy refers to a difference in leg length, which can cause gait abnormalities, back pain, and joint stress. Causes of Limb length discrepancy can be congenital, developmental, post-traumatic, post-infective, or neoplastic. The treatment depends upon the condition and age of the child.
5. Developmental Dysplasia of the Hip (DDH):
The Hip joint is a ball and socket joint. The femoral head forms the ball, and the acetabulum forms the socket. The socket is generally deep and cup shaped to allow the ball to sit in. DDH is a spectrum of hip conditions that includes shallow socket (dysplasia), ball is partiallyout of the socket (subluxation) to a completely separated ball and socket joint (dislocation)
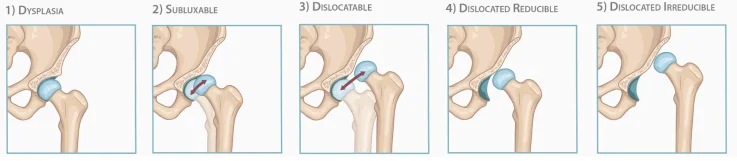
It is essential to diagnose and treat DDH at an appropriate age, since untreated children often land up undergoing multiple hip surgeries. Untreated children of dislocated hips often have shorter leg of the affected side and walk with a limp. They also develop hip pain, back pain and knee pain as these joints get affected.
DDH can develop even in older children.
How to Diagnose DDH
Risk factors
- First child – often at a higher risk for developing DDH
- Breech – when the child is NOT born head first
- Family History – Higher risk of the child having DDH if family member has had
it. - Intra-uterine overcrowding – large baby, twin pregnancy, oligohydramnios
- Other Congenital conditions – clubfoot, spine anomalies, torticollis, foot
deformity, lower limb deformity
Clinical signs
- Limited abduction – if the parent complains of having difficulty in putting diapers, is unable to spread the thighs equally.
- Difference between both legs – if one leg appears shorter than the other, or there are abnormal thigh folds.
- Limp – the child walks with a painless limp
- Clinical examination – the orthopaedic surgeon examines the child’s hips. Tests such as Ortolani and Barlow test, Klisic sign, telescopy test, Galeazzi test are done to find out whether the child has DDH
Tests
- Ultrasound (Sonography) – the best way to diagnose in a child less than 6 months old.
- Xrays of the hips
TREATMENT
The treatment of every child depends on age of child and severity of dislocation.
Upto 6 months – the treatment depends on the severity of DDH. If the hip is reducible – a Pavlik Harness – a belt – is used that helps keep the hip within the joint. Repeat ultrasounds are done to make sure the hip is within the joint. It is important to be compliant with the belt – failure to do so leads to surgery.
6 months to 1 year – Small surgery in the form of closed reduction, arthrogram and
hip spica cast is done to keep the hip inside the joint. This procedure is done under
general anaesthesia.
Above 1 year – The child generally requires surgery under anesthesia. The type of surgery depends upon whether the socket is also involved. The surgery done is open reduction – where the hip joint is opened and the ball is put back into the socket. Sometimes the shape of the socket needs to be changed so that the joint is stable 0 which is called acetabuloplasty.
6. Slipped Capital Femoral Epiphysis:
The Hip joint is a ball and socket joint. The femoral head forms the ball, and the acetabulum forms the socket. The femoral head has a growth plate from where the head grows. SCFE is a condition when the growth plate is weakened, and the ball (head) slips downward and backward. This condition often occurs in adolescents.
It is generally more common in boys, who are obese. There may or may not be a history of
trauma. The most common complaint is hip pain, limp, and change in the way of walking.
The child is either unable to walk or walks with feet turned outwards.
Xrays of hips are done.

Sometimes a CT scan or MRI may be required.
Treatment is in the form of Surgery. There is no non operative treatment for SCFE. The surgery depends on the severity of the slip.
Percutaneous in-situ screw fixation – often done in mild slips. One or two screws may be used to prevent further slippage.

(Percutaneous Screw Fixation)
Modified Dunn Osteotomy – involves opening the hip joint and putting the head back into
place. The head is then fixed with wires and screws. It is often done in moderate and severe
slips.
Complications
Avascular necrosis – stoppage of blood supply of the femoral head. This is common in patients who have suffered SCFE. This causes the head (ball) to collapse and generally requires further treatment.
Chondrolysis
Osteoarthritis
7. Perthes diseases of the hip - Legg Calve Perthes Disease (LCPD):
Perthes disease is idiopathic avascular necrosis of the femoral head (ball). The ball slowly collapses – which causes pain, limp, and loss of movement of the hip joint.

Xrays and MRI are needed to diagnose Perthes and to find out the severity of the disease. Treatment depends on the age of the child, and stage of the disease.
8. Tibial Bowing:
Tibial bowing is a condition when the calves / shin of the baby are bowed or curved. It is generally present only in the leg area. The bow can either be backwards, outwards or inwards. It represents congenital abnormality in the leg (congenital pseudarthrosis of tibia, posteromedial bowing of tibia, fibula hemimelia) and needs to be monitored and may require surgical treatment.
9. Clubfoot

Clubfoot, also known as congenital talipes equinovarus, is a relatively common congenital deformity that affects the positioning of a child’s foot or feet. Children with clubfoot are born with one or both feet turned inwards and downwards, making it challenging for them to walk or wear regular shoes. Early diagnosis and intervention are crucial to ensure the best outcome. Clubfoot can be idiopathic, atypical, or syndromic, and treatment depends on the type of clubfoot. Clubfoot has a high rate of relapse and must be followed up long term to catch early recurrence. Even after treatment compliance, recurrence is known to occur and may warrant intervention at a later date.
Non-Surgical Treatment: The gold standard for non-surgical treatment of clubfoot is the Ponseti method. This approach involves gentle manipulation and casting to gradually correct the foot’s position. Once a satisfactory foot position is achieved, the last step is to correct the tight heel cord, which may be done with a tenotomy. After the correction, the child is fitted with a foot abduction brace to maintain the corrected position and promote proper development. The child wears the foot abduction brace till the age of 3-4 years.
Surgical Treatment: Surgical intervention is reserved for cases where non-surgical methods do not yield the desired results. It may involve a minor procedure to lengthen the Achilles tendon or, in more complex cases, extensive surgery to reposition bones and tendons
10. Congenital Vertical Talus
Congenital vertical talus (CVT), also called rocker bottom foot, is another congenital foot deformity that affects a child’s ability to walk and maintain proper foot arches. Unlike clubfoot, CVT presents with an upward and backward arch of the foot, making it resemble a rocker bottom. CVT has a high rate of relapse and must be followed up long term to catch early recurrence.
Non-Surgical Treatment: Non-surgical treatment options for congenital vertical talus are limited. After the initial diagnosis, trial of casting in children is done. Serial casting for deformity correction is done with plasters being changed on a weekly basis. Children are often fitted with orthotic devices like ankle-foot orthoses (AFOs) to support the foot and maintain the corrected position. However, these measures are typically used in conjunction with surgical intervention.
Surgical Treatment: Surgical treatment is the primary approach for congenital vertical talus. It can be done with serial casting, thereby reducing the quantum of surgery required. Reduction and pinning of the talo-navicular joint in the corrected position, followed by casting can be done in cases where the joint alignment is maintained. However, the treatment of congenital vertical talus can involve surgical procedures including but not restricted to tendoachilles lengthening, dorsal release of tendons or an extensive soft tissue release. The procedure involves repositioning the bones and tendons to correct the deformity. Post-surgery, physical therapy and orthotic devices are essential to maintain proper alignment and function.
11. Flatfeet

Flatfeet, or pes planus, is a common paediatric foot condition in which the arches of one or both feet do not develop as expected. Most children have flatfeet in early childhood, but it typically resolves as they grow. Some cases, however, persist and may lead to discomfort or pain. Flatfoot can be flexible or rigid. Treatment of flatfoot is dependent on the patient’s symptoms and underlying condition.
Non-Surgical Treatment: Non-surgical treatment options for flatfeet focus on alleviating discomfort and promoting proper development. Custom orthotics or shoe inserts, along with exercises to strengthen the muscles that support the arch, are commonly recommended. Proper footwear with adequate arch support is also crucial.
Surgical Treatment: Primary patients who undergo surgery are – symptomatic flexible flatfeet, rigid flatfeet, and syndromic children (ex. Cerebral Palsy, Arthrogryposis). Surgical intervention for flatfeet is relatively rare and is typically reserved for severe cases that do not respond to non-surgical treatments. Surgical options may involve realigning or fusing specific foot bones to create or restore the arch.
12. Toe Walking
Toe walking is a gait pattern in which a child consistently walks on their toes rather than their whole foot. It can be associated with various conditions, including cerebral palsy and autism, but can also occur without an underlying disorder.
Non-Surgical Treatment: Non-surgical treatments for toe walking are typically the initial approach. Physical therapy plays a central role in these treatments, focusing on stretching and strengthening the calf muscles. Orthotic devices, such as night splints, may be recommended to encourage flat-footedness while sleeping.
Surgical Treatment: Surgical intervention is only considered for severe and persistent cases. Procedures like tendon lengthening or release may be necessary to address overly tight calf muscles contributing to toe walking.
13. Metatarsus Adductus
Metatarsus adductus is a condition in which a child’s forefoot is turned inward relative to the hindfoot. The foot looks to be bean shaped. It can make walking difficult and cause discomfort in some cases.
Non-Surgical Treatment: Non-surgical treatments are often successful in correcting metatarsus adductus. Stretching exercises and orthotic devices like splints or specialized shoes can be employed to address the condition. Serial casting may also be used for more severe cases.
Surgical Treatment: Surgical intervention is rare and is usually reserved for cases where non-surgical methods fail to correct the deformity.
14. Congenital Toe Deformities
Congenital toe deformities encompass a wide range of conditions, such as webbed toes, extra toes, or crooked toes. These deformities can be minor or more complex, but they can all affect a child’s comfort and self-esteem.
Non-Surgical Treatment: Non-surgical approaches vary depending on the specific congenital toe deformity. Some milder cases may benefit from physical therapy or splinting to encourage proper development and function.
Surgical Treatment: Surgical correction is often necessary for more complex congenital toe deformities, including webbed toes or extra digits. The surgical procedures aim to release, realign, or reconstruct the affected toes.

(Congenital Toe Abnormalities in Children)
