Brain and Spine tumours
Medical Laboratory And Specialists Services
Brain tumours arise from the various different parts of the brain in different areas of the brain and depending on their nature and region of involvement, they present with different features such as headache, hemiparesis, seizures, visual disturbances, and speech disturbances to name a few. Their treatment outcomes depend upon the location and the grading or molecular typing of the tumour.
Our philosophy:
- Not all tumours need surgery. Many small tumours such as small meningiomas, small focal gliomas, small schwannomas, small colloid cysts, pituitary adenomas, and epidermoid cysts may be just incidental findings on imaging. They may be managed by just medication and observation, and a large proportion of these lesions never grow in size enough to ever warrant surgery. We, at Dr. Bansals Arogya Hospital understand that our goal is to treat the patient and not just the tumour and hence, we offer our services judiciously with due consideration.
- Not all Brain tumours are fatal. Many of the brain tumours as we describe ahead are benign tumours which can be surgically cured. Our expertise helps us to guide you in understanding your disease and we assist our patients in living a life beyond their disease.
- Quality of life is as important as duration of life. Many brain tumours and their surgery need the surgeon to make a choice to determine which functional areas of the brain are necessary to be preserved and which can be sacrificed. We discuss with our patients their possible options and provide the best functional outcomes for the best possible quality of life.
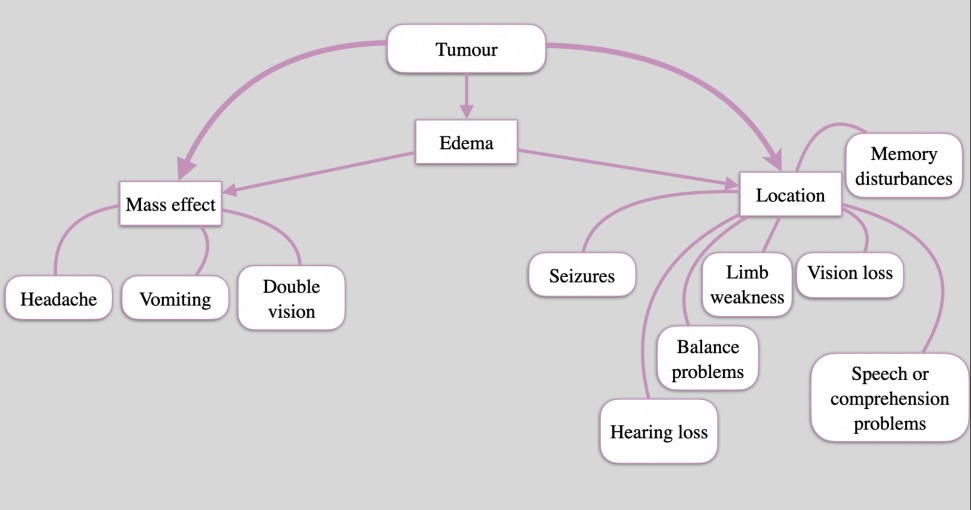
( Understanding the Symptoms of Tumours )
Meningiomas:
They are tumours that arise from the arachnoidal cap cells usually as a part of the dura mater (Protective layer around the brain and spine). They cause deficits by compressing brain or spine parenchyma and causing vascular changes in the underlying brain or spinal cord. Meningiomas are usually benign and rarely malignant. Complete resection of the meningioma, surrounding dura and bone has a 10 year recurrence rate of less than 10%. Higher grade, atypical or anaplastic meningiomas have a higher rate of recurrence.
They usually warrant surgical excision but some small meningiomas may never grow
and can just be observed. Smaller meningiomas in difficult to access locations may also
be treated with radiation therapy.
Schwannomas:
Schwannomas are benign tumours that arise from the cells in the sheath surrounding the axons of nerves. They may arise in the brain, spine or on any nerve in the body. They are slow growing and cause deficits either due to compression or direct injury to nerve. They can be surgically resected, giving radiotherapy or just be observed if they are small.
Vestibular schwannomas or acoustic schwannomas are commonly seen schwannomas
that cause hearing loss, imbalance, facial numbness, taste impairment, headaches, and
facial weakness most often. They are excised by skull base surgeons and usually have
a good outcome with excellent survival. Small tumours may be treated by gamma knife
radio surgery and have excellent outcomes.
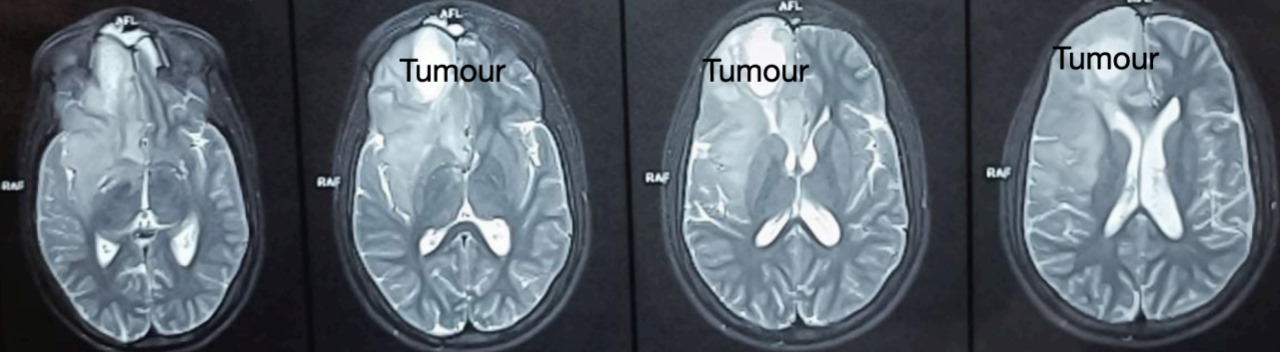
Gliomas:
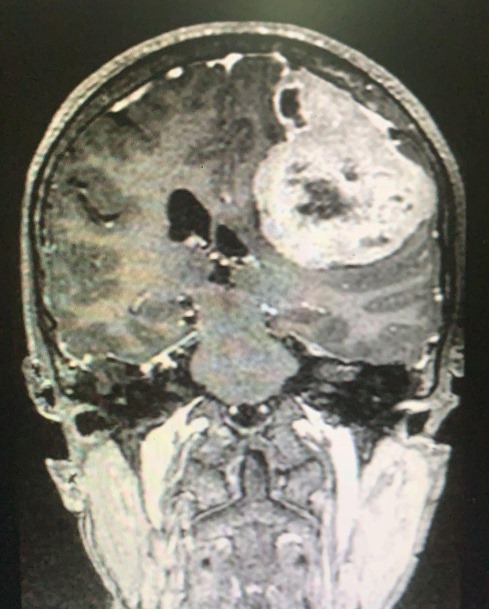
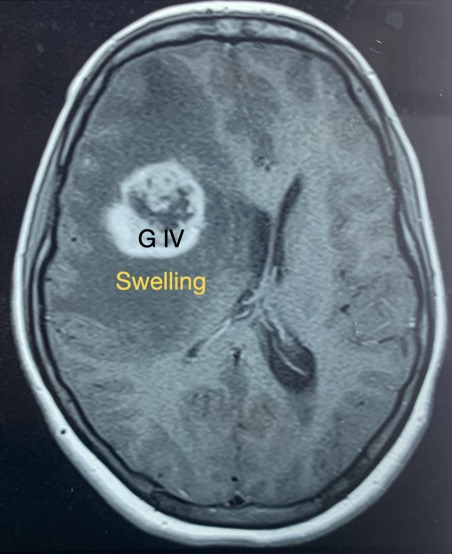
They are tumours that arise from the glial brain and spinal cord cells. Hence, these tumours tend to cause effects by either directly damaging functional areas of the brain or compressing the structures. They vary in grades from 1 to 4, which denotes their ability to recur and spread into surrounding areas. Grade 1 tumours have generally less recurrence and less invasiveness into surrounding areas. Grade 2 and 3 tumours have a higher degree of invasiveness and recurrence rates. Grade 4 tumours are high grade tumours that almost universally recur and have a high degree of invasion into surrounding brain matter. Amongst grade 2/3 tumours, Oligodendrogliomas are a variety of tumours that have a good response to radiotherapy and chemotherapy.
Most common gliomas are astrocytomas that arise from astrocytes. These are cells that
support the neuronal cells by providing them with nourishment, support and an environment to optimally function. These tumours can affect patients based on their size and area that they involve and can cause a large variety of clinical features.
They can be surgically treated using a wide array of tools such as intraoperative ultrasound, neuro-navigation, awake monitoring and intraoperative fluorescence to effectively delineate and safely remove these tumours. Not all tumours are completely removable as it may lead to injury of an area controlling an important function such as sleep, power in the limbs or behavioural changes. In such cases, a maximal safe resection is done. There are other treatment options after surgery or in cases where surgery is difficult such as radiotherapy and chemotherapy.
Other newer treatment options such as TTFields, Immunotherapy, Laser interstitial thermal therapy, and focused ultrasound are also being explored but with limited vailability in India.
Grade 4 Glioma (Old Name Glioblastoma Multiforme)
Grade 3 Oligodendroglioma Medulloblastomas
(Grade 3 Oligodendroglioma)
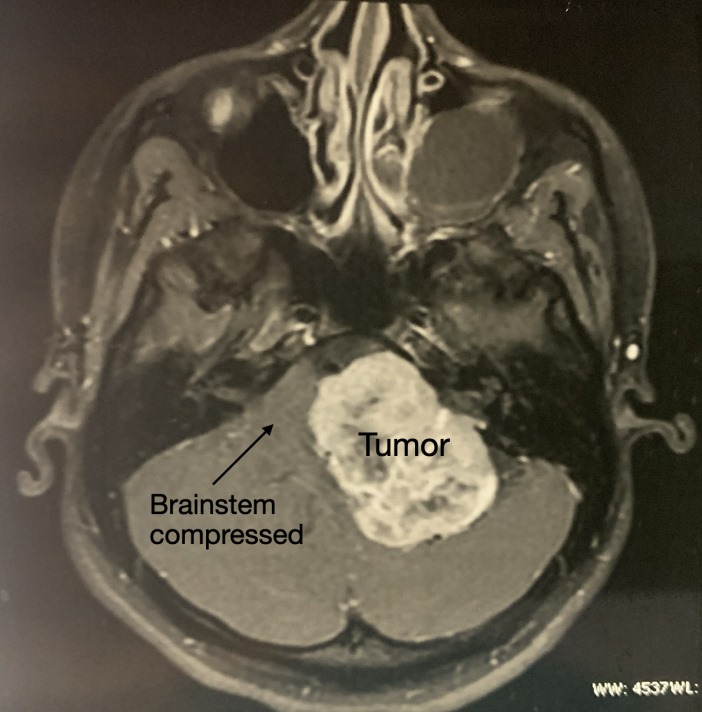
These are tumours commonly seen in children and young adults. They are high grade tumours, with varied recurrence rates depending on the specific group type of the tumour which is known after histopathological analysis and immunohistochemical analysis of the tumour.
They are usually seen in the posterior fossa and are treated by surgery along with radiation and chemotherapy. Complete resection of the tumour is always the goal in such tumours. But in cases invading the brainstem, limited resection may be considered.
Surgery gives very good results and patients may have minor difficulties in fine and skilled tasks for some time. In some children with posterior fossa tumours, inability to speak develops for some time after surgery known as cerebellar mutism. This generally resolves over time in most cases.
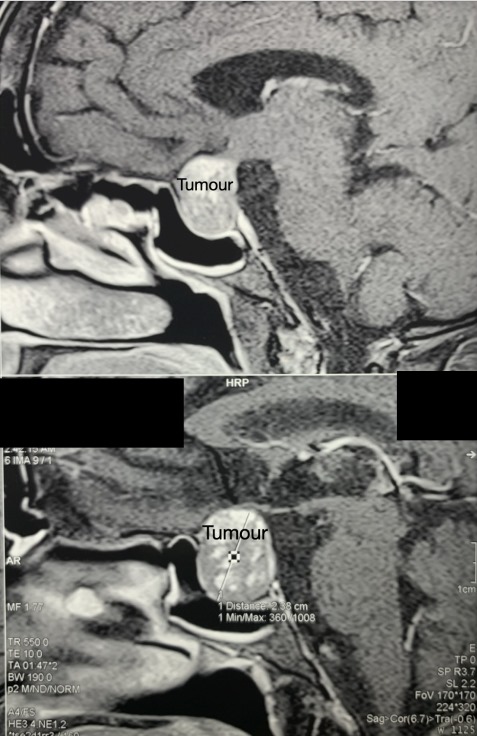
Pituitary adenomas:
These are common brain tumours seen in adults. They arise from the pituitary gland, and the master endocrine gland, and may be functional adenomas or non-functional adenomas.
- Non-Functional pituitary adenomas are primarily treated by a skull base surgeon. Patients with these tumours present with symptoms due to the tumour pressing on surrounding structures such as headache, double vision and visual loss. There may be symptoms due to a deficiency of hormones such as lethargy, somnolence, galactorrhea, loss of libido and infertility. They are typically treated by surgery and we endoscopically remove the tumour through the nose. In large tumours, radiation may be needed to destroy the tumour that is surgically unsafe to remove. These surgeries are very rewarding with good visual recovery in most patients.
- Functional pituitary adenomas are tumours that secrete excess of hormones which are synthesised by the pituitary gland.
Growth hormone secreting:
Patients whose tumours secrete the human growth hormone present with gigantism or acromegaly. Gigantism occurs when there is excess secretion at a young age. It results in an abnormally tall person with large stature, large hands, big tongue, prominent jaw and forehead. Acromegaly occurs when there is excess secretion after the growth is completed. These patients present with large hands, a big tongue, a prominent jaw and forehead, coarsening of skin and facial features. While the cosmetic changes may be alarming, they aren’t the main problem in this disease.
These patients have a high risk of developing heart problems, elevated blood pressure and diabetes mellitus. The lifespan of a person with such tumours is decreased by at least 10 years if left untreated. Surgical excision is an excellent option for the treatment of such tumours and most tumours can be treated by endoscopic excision through the nose. Other options such as control through medication and radiation are adjuvants that help patients live a near normal life. Most cosmetic features of acromegaly, as mentioned above, are reversed after adequate control of the disease.
Cushings disease:
Cushings disease refers to an excess of cortisol hormone as a result of a tumour in the pituitary gland. Cushings syndrome has the same features but the source of cortisol or ACTH is elsewhere. The pituitary gland produces a hormone known as ACTH(Adreno-cortico-trophic Hormone) which stimulates the adrenal glands to produce cortisol. Cortisol is an emergency response hormone. When the tumour results in excess production of ACTH, there occurs an excess of cortisol secretion from the adrenal glands. This results in a large number of features as shown in the picture. There is associated difficulty in controlling elevated blood pressure and difficulty in controlling diabetes mellitus.
The diagnosis is done with the expertise of an endocrinologist to rule out other causes of the excess cortisol. Tests such as Dexamethasone suppression test and inferior petrosal sinus (blood vessel that drains blood from the pituitary gland) sampling assist in confirming the source of the disease. MRI of the pituitary gland helps in locating the exact site of the tumour.
Surgery through an endoscopic trans-nasal approach remains the most effective treatment option with a high chance of cure of the disease. As these tumours are usually small, it needs a skilled surgeon to identify the tumour and precisely excise it while causing minimal damage to the surrounding normal pituitary gland.
Medication is needed to control the disease enough to make the patient fit for surgery and also in cases where surgery is unable to completely remove the tumour. Radiation also assists in the control of this disease in case of recurrence or residual disease.
Prolactinomas:
These are tumours of the pituitary gland that cause an excess secretion of the hormone prolactin. This hormone is mainly responsible for the secretion of milk from the breast in a new mother. They present differently in men and women. The clinical features are seen in the photos shown.
These tumours are most commonly treated by an endocrinologist and are usually amenable to medication such as Cabergoline or Bromocriptine. Most patients have great responses to medication with reversal of the disease symptoms within a couple of months after achieving the appropriate dosage needed.
However, surgery is needed in some cases.
- In patients with large tumours causing visual disturbance or visual loss, surgery is needed in order to protect the vision.
- In patients with tumours unresponsive to medication.
- In patients unable to tolerate the medication.
- In patients who develop CSF leak as a result of the shrinkage of tumour after medication.
Depending on the size and growth of the tumour, different surgical approaches may be used. The endoscopic trans-nasal approach remains the most commonly used approach with good results. Surgery for prolactinoma has a good outcome in general. Radiation has a limited role in the treatment of prolactinomas.
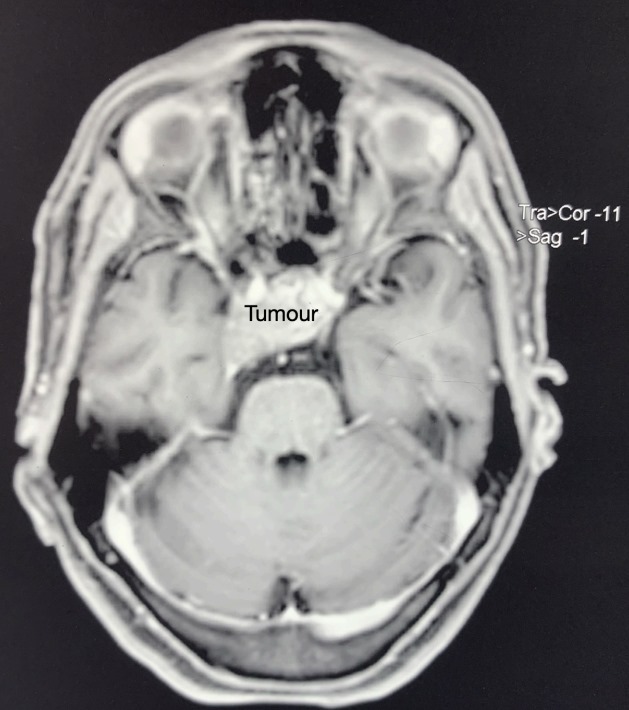
Craniopharyngiomas:
These are uncommon tumours which arise from cells that were trapped in the brain and stuck in the wrong location when the brain and nose were developing in the mother’s womb. These tumours are typically benign lesions in a dangerous location. They tend to grow and stick to the surrounding brain, pituitary gland, blood vessels and nerves. Due to their tendency to stick to surrounding vital structures, they are difficult to remove completely and have a tendency to recur.
They cause problems like headaches, vision problems, double vision, vomiting, drowsiness, seizures, excessive appetite or complete loss of appetite, and excessive urine. They may also cause hormonal problems due to pressure on the pituitary gland or its stalk. The treatment for this tumour is first to stabilise the effects caused by the tumour and then excise the tumour. Excision can be done endoscopically or by open surgery depending on the location and size of the tumour.
Surgery is essential for both the diagnosis and treatment of this tumour. Following
surgery most cases need radiotherapy and additional treatment by an endocrinologist. Recovery is good and patients can lead a normal life with the appropriate medication.
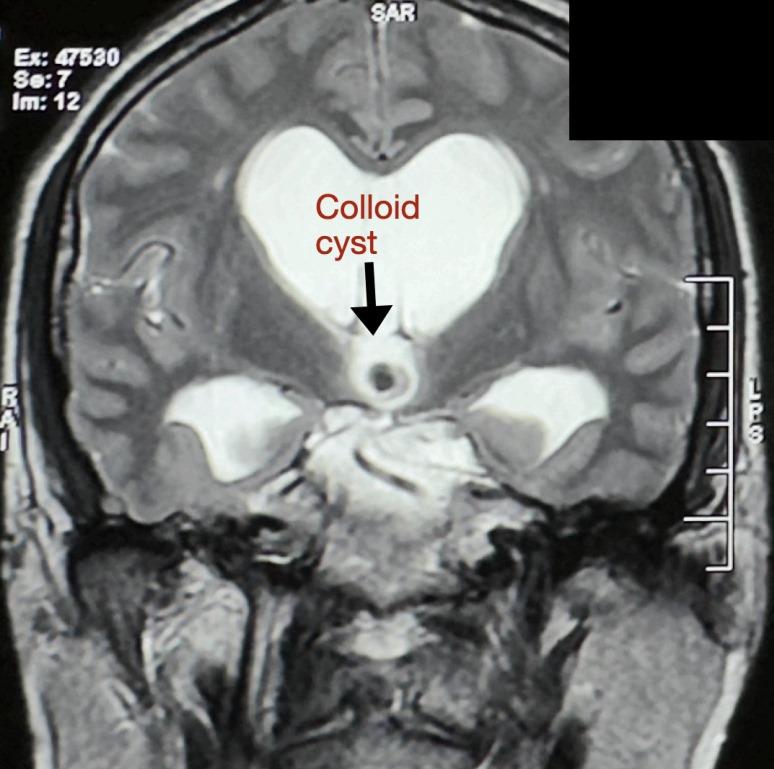
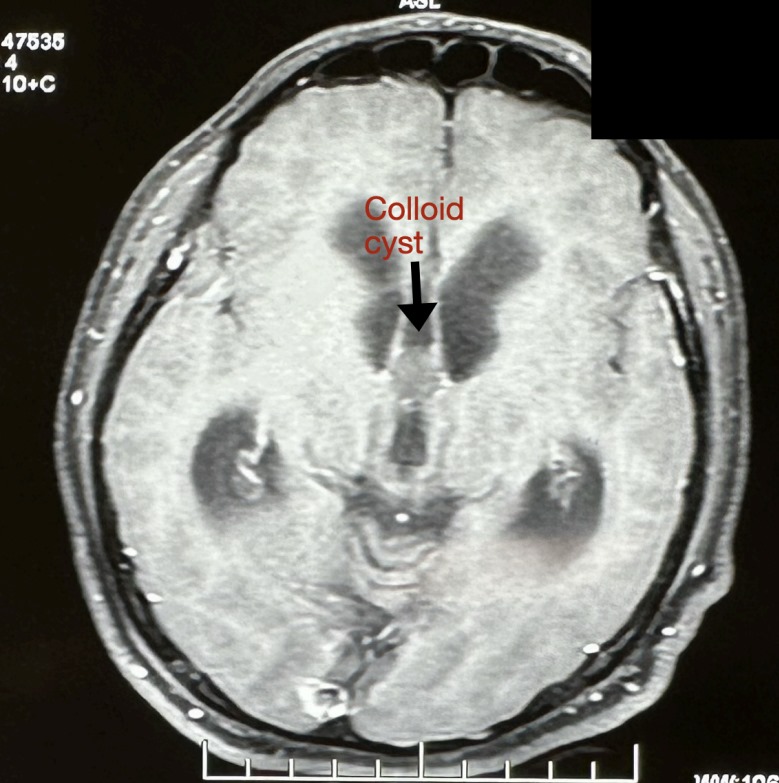
Colloid Cyst:
These are small cystic benign tumours that arise from cells that get trapped within the brain during the early formative years of the brain. They form a small cystic lesion at dangerous locations and have a tendency to block the flow of CSF from the two large lateral ventricles through the foramen of Monroe into the thin and smaller third ventricle of the brain. This leads to headaches and vomiting usually with visual blurring.
The sudden blockage of CSF causes the ventricles to dilate and compress and stretch the areas controlling the legs which leads to ‘drop attacks’. These are attacks of sudden weakness of the legs which leads to falls. Large cysts or cysts in dangerous locations need to be excised as an emergency as they may lead to blockage which can be life threatening.
Surgery may be done endoscopically or as a small open surgery. Endoscopic surgery has a higher recurrence rate when compared to open surgery and hence is reserved for limited cases only. Surgery has good outcomes and it is one of the most rewarding surgeries with a complete cure possible.
Why Choose Dr. Bansals Arogya Hospital for Brain and Spine Tumour Surgery?
Dr. Bansals Arogya Hospital is committed to providing exceptional care for patients with brain and spine tumours. Here’s why our hospital is the preferred center for this highly specialized surgery:
- Expertise and Experience:
Our neurosurgical team comprises some of the most experienced and skilled surgeons in the field of brain and spine tumour surgery. With extensive training and a history of successful procedures, our experts are equipped to handle the complexities of these delicate surgeries with precision and confidence. - Advanced Technology:
We utilize cutting-edge technology and the latest surgical techniques to ensure the best possible outcomes for our patients. Our hospital is equipped with state-of-the-art operating rooms, advanced imaging systems, and minimally invasive surgical tools, all designed to enhance the accuracy and safety of tumour removal. - Multidisciplinary Approach:
Our multidisciplinary approach brings together specialists from neurosurgery, oncology, radiology, and rehabilitation to provide comprehensive care. This collaborative effort ensures that all aspects of your health are considered, from diagnosis to treatment and recovery, offering a holistic treatment plan tailored to your needs. - Personalized Treatment Plans:
Every patient is unique, and so are their medical needs. We develop individualized treatment plans based on thorough evaluations and consultations. Our personalized approach ensures that you receive the most effective treatment tailored specifically to your condition and overall health goals. - Exceptional Patient Care:
Patient care is at the heart of everything we do at Dr. Bansals Arogya Hospital. Our compassionate medical team is dedicated to supporting you throughout your journey, from pre-operative preparations to post-operative recovery. We provide continuous support, education, and resources to help you and your family navigate the treatment process. - Proven Success:
With a high success rate in brain and spine tumour surgeries, Dr. Bansals Arogya Hospital has established a reputation for excellence. Our commitment to delivering superior medical care is reflected in the positive outcomes and satisfaction of our patients. - Comprehensive Rehabilitation:
Post-surgery recovery is crucial, and our comprehensive rehabilitation programs are designed to help you regain your strength and functionality as quickly and safely as possible. Our team of physiotherapists and occupational therapists work closely with you to create a personalized rehabilitation plan that supports your recovery journey.
Choosing Dr. Bansals Arogya Hospital for your brain and spine tumour surgery means entrusting your care to a team that prioritizes your health, recovery, and well-being. We are dedicated to providing expert surgical care, advanced technology, and compassionate support to help you overcome your health challenges and achieve the best possible outcomes. Your path to recovery starts with us.
