Traumatic Brain Injury
Medical Laboratory And Specialists Services
As an experienced neurosurgeon, I understand the complexities and challenges that come with traumatic brain injury (TBI). This page is designed to provide you with comprehensive information about TBI, including different types of intracranial hemorrhages, concussive head injury, and diffuse axonal injury, along with their causes, symptoms, diagnosis, treatment options, and recovery process.
Understanding Traumatic Brain Injury (TBI)
Traumatic brain injury refers to any sudden, external force that causes damage to the brain. This can result from various incidents such as falls, car accidents, sports injuries, or violent assaults. TBIs can range from mild (concussion) to severe, and their effects can be temporary or long-lasting.
Common Causes of TBI
- Falls, especially among older adults and children
- Motor vehicle accidents
- Sports-related injuries, such as concussions in football or soccer
- Assaults or violence
Symptoms of TBI
The symptoms of TBI can vary depending on the severity of the injury. Common symptoms include:
- Headaches
- Confusion or disorientation
- Memory problems
- Dizziness or balance issues
- Nausea or vomiting
- Sensory changes (blurred vision, ringing in ears)
- Mood changes (irritability, depression, anxiety
It’s important to seek medical attention if you or someone you know experiences any of these symptoms after a head injury.
Diagnosis of TBI
Diagnosing TBI often involves a combination of physical exams, neurological assessments, imaging tests (such as CT scans or MRIs), and evaluation of symptoms and medical history.
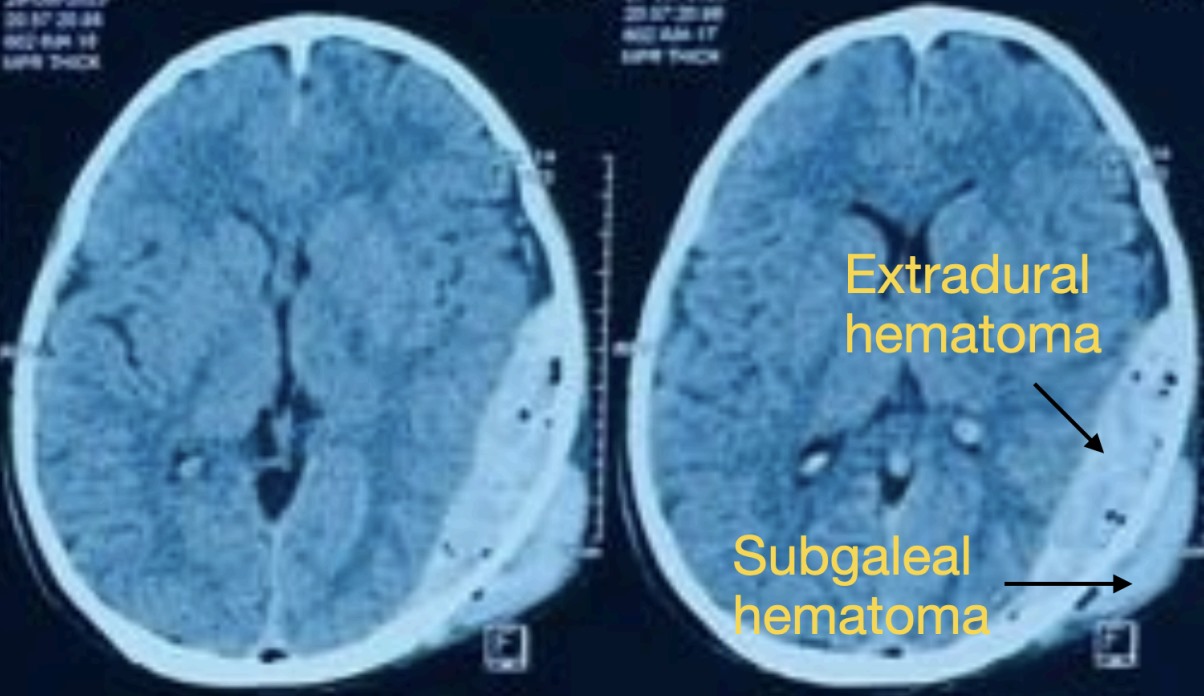
Types of Intracranial Hemorrhages in TBI
Intracranial hemorrhages refer to bleeding within the skull. They can occur in different areas of the brain and have specific characteristics:
1. Epidural Hematoma (EDH):
Bleeding between the skull and the outer layer of the brain (dura mater). Symptoms can include headache, dizziness, confusion, and focal neurological deficits. It has the best prognosis.
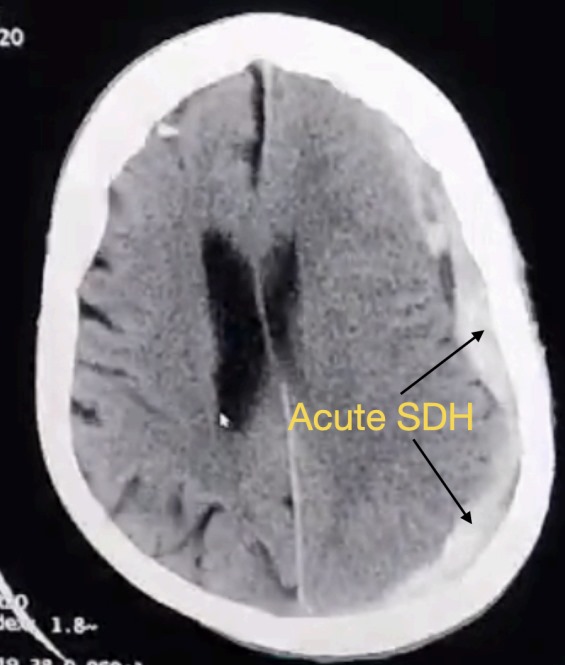
2. Subdural Hematoma (SDH):
Bleeding between the dura mater and the arachnoid mater (a membrane surrounding the brain). Symptoms may include headache, altered mental status, weakness, and seizures. It has a good prognosis when only subdural hematoma is present.
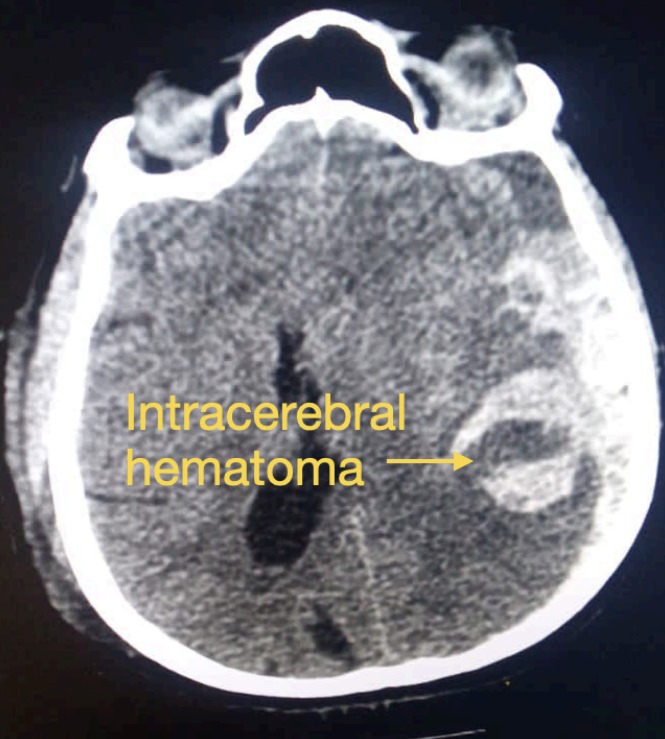
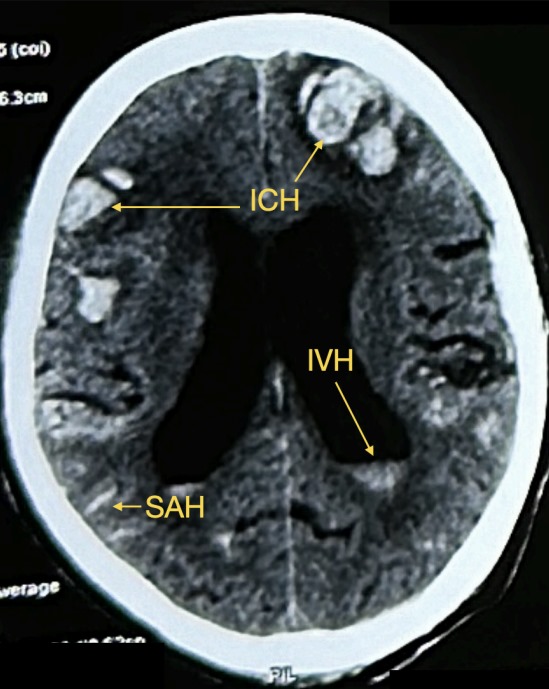
3. Intracerebral Hemorrhage (ICH):
Bleeding within the brain tissue itself. Symptoms depend on the location and size of the hemorrhage and may include headache, weakness, numbness, speech difficulties, and loss of consciousness. It indicates that damage has already occurred within the brain tissue and has the worst prognosis overall.
4. Subarachnoid Hemorrhage(SAH):
Bleeding in the space between the arachnoid membrane and the brain surface. It can cause sudden severe headache, nausea, vomiting, and neurological deficits. It usually occurs in conjunction with one of the above types of hemorrhage and indicates a higher severity of brain injury.
Concussive Head Injury
A concussion is a mild form of TBI that often occurs after a blow to the head or a sudden jolt to the body. Symptoms of a concussion can include headache, dizziness, confusion, memory problems, sensitivity to light or noise, and changes in mood or behavior. Most concussions resolve with rest and gradual return to normal activities, but some cases may require medical
evaluation and management.
Diffuse Axonal Injury
Diffuse axonal injury (DAI) is a severe form of TBI characterized by widespread damage to nerve fibers (axons) in the brain. It often results from rapid acceleration or deceleration forces, such as those seen in car accidents or high-impact sports injuries. DAI can lead to coma, cognitive deficits, motor impairments, and long-term disabilities. Treatment may involve surgery, rehabilitation, and supportive care.
Subgaleal Hematoma:
Bleeding between the skull bone and the overlying scalp is known as subgaleal hematoma. It is not significant in adults unless infected. In infants and young children a subgaleal hematoma may cause significant loss of blood, hence it must be addressed at the earliest.
Treatment Options
Treatment for TBI depends on the type and severity of the injury. It may include rest, pain management, monitoring for changes in symptoms, surgery to relieve pressure or control bleeding, rehabilitation programs, and supportive therapies to promote recovery and improve quality of life.
Most surgeries for traumatic brain injury involve the removal of the skull bone and evacuation of
the blood clot. Most of the time, the skull bone is immediately placed back and fixed. In some cases the bone may be kept separately until the brain swelling reduces and the patient is stable. This procedure is known as decompressive craniectomy. The bone is replaced with another surgery after 6 – 10 weeks.
Cranioplasty
What is Cranioplasty?
Cranioplasty is a surgical procedure designed to repair and reconstruct defects or deformities in the skull. These defects can result from trauma, surgical interventions, congenital anomalies, or diseases that affect the cranial structure. By restoring the shape and function of the skull, cranioplasty not only improves the cosmetic appearance but also offers crucial protection to the underlying brain tissue.
Why is Cranioplasty Performed?
Cranioplasty is performed for several reasons:
- Protection of the Brain: Openings or defects in the skull can expose the brain to
potential injuries. Cranioplasty provides a protective barrier. - Cosmetic Improvement: Skull deformities can affect a person’s appearance, leading to psychological and social challenges. Cranioplasty can restore a more natural look.
- Neurological Improvement: Some patients experience neurological improvements after cranioplasty, including better cognitive function, reduction in headaches, and alleviation
of other neurological symptoms.
Materials Used in Cranioplasty
Various materials can be used for cranioplasty, each with its advantages:
- Autologous Bone: Using the patient’s own bone, usually harvested during the initial
surgery. This method reduces the risk of rejection and infection. - Alloplastic Materials: Synthetic materials such as titanium, polymethyl methacrylate (PMMA), and polyetheretherketone (PEEK). These materials are durable, biocompatible, and can be custom-shaped to fit the defect perfectly.
Risks and Complications
As with any surgical procedure, cranioplasty carries certain risks:
- Infection: Although rare, infections can occur and may require additional treatment or surgery.
- Implant Rejection: The body may reject synthetic materials, leading to inflammation or other complications.
- Hematoma: Accumulation of blood at the surgical site, which may need drainage.
- Neurological Symptoms: Temporary or, in rare cases, permanent neurological symptoms can occur.
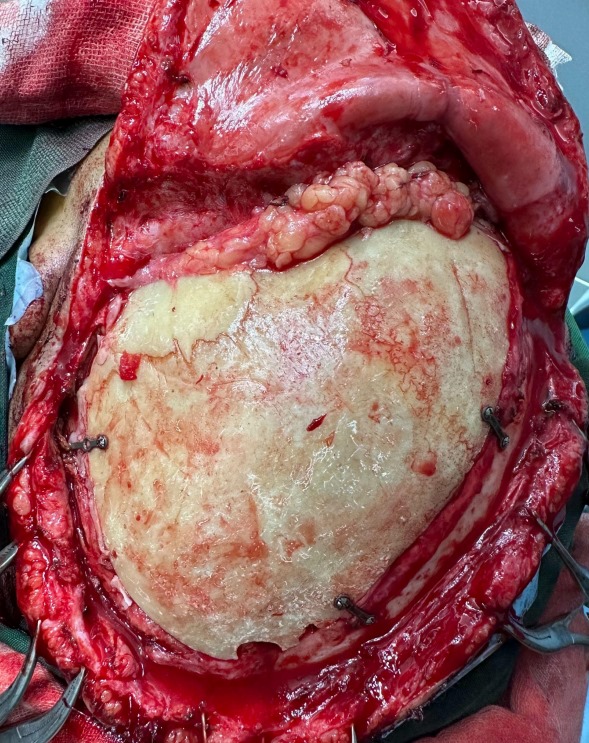
(Post autologous cranioplasty after decompressive craniectomy for traumatic brain injury)
Recovery and Rehabilitation
Recovery from TBI can be a gradual process and may involve various healthcare professionals,
including neurosurgeons, physical therapists, occupational therapists, speech therapists, and psychologists. Rehabilitation programs focus on improving cognitive abilities, motor skills,
emotional well-being, and overall function.
Why Choose Our Neurosurgery Practice?
At Dr. Bansals Arogya Hospital, we specialize in the diagnosis, treatment, and management of
traumatic brain injuries, including intracranial hemorrhages, concussive head injuries, and
diffuse axonal injuries. Our team of experienced neurosurgeons, nurses, therapists, and support staff is dedicated to providing personalized, compassionate care to help patients achieve optimal recovery and quality of life.
Our Services Include:
- Comprehensive TBI evaluations and treatment plans
- Minimally invasive neurosurgical procedures
- Neurorehabilitation programs tailored to individual needs
- Patient and family education and support
- Collaborative care with other healthcare professionals
Contact Us Today
If you or a loved one has experienced a traumatic brain injury or if you have any concerns about brain health, we’re here to help. Contact us to schedule a consultation or learn more about our services.
